How to Get Rid of a Scar on Your Lip
Dentists routinely see patients who are suffering from trauma to the lips. If we do not personally treat and suture these patients' lips ourselves, we are at least witness to a significant amount of lip and perioral scarring which formed subsequent to previous trauma. Most injuries to the facial structures seen in the emergency room are related to the soft-tissue of the lip and perioral area (62.8%). 1,2 A majority of these traumas are suffered by children. 3,4 In most instances, patients who have suffered lip and perioral soft tissue trauma are treated without regard for potential unaesthetic scarring. 5 Postsuturing revisionary surgery can be complicated and may involve more scar tissue. With the advent of newer aesthetic materials, and minimally invasive cosmetic procedure (MICP), lip and perioral scar revision can be treated in the dental office with local anesthetic in a short sequence of treatments.
|
INTRODUCTION
Many methods have been used to relieve lip and perioral scarring including chemotherapy, and surgical/nonsurgical procedures. Since the advent of modern day MICP procedures, a significant number of scars around the lip and perioral may be treated in the office with little or no down time. 6 Techniques such as subcision, dermal fillers, and ablative laser therapy have been successfully used. The combination of subcision and immediate dermal filler placement can present advantages to treatment. In addition, laser ablative treatment for a final cosmetic treatment results in a marked reduction in scar appearance.
This article will demonstrate the use of a combination method of needle subcision and filler placement to reduce mild to moderate lip and perioral traumatic scarring. In addition, fractional laser ablative treatment on upper lip (Zone A) to enhance scar cosmesis will be demonstrated. The Gordon lip and perioral classification for the treatment template will be used.
GORDON CLASSIFICATION (CLASSIFICATION SYSTEM DESCRIPTION)
Maxillary Labial
Zone A (ZA) extends from, and includes, the superior aspect of the vermilion border to the lower border of the columella nasi of the nose. This zone is wider due to the philtrum that is, at times, augmented in this zone. Zone B (ZB) is the area midpoint between the inferior border of the vermilion border (ZA) and the superior border of Zone C (ZC). ZC is the area from the inferior border of ZB to the lower transitional zone (wet/dry line) lip (Figures 1 and 2).
Mandibular Labial
ZC extends from the transitional zone (wet/dry line) to the border of ZB. ZB extends from the middle of the lip (border of ZB) to the vermilion border of the lower lip. ZA extends from, and includes, the vermillion border and the cleft, superior to the metal protuberance of the chin. Classification I, which applies to the lip and perioral area, is a template (or a border) that defines an area of treatment with MICPs. The Gordon Classification maps the lip and perioral area in order to facilitate communication, teaching, and recording of treatment.
CASE REPORT
Diagnosis and Treatment Planning
A female patient presented to our practice on a routine dental visit (Figures 3 and 4). The patient was asked about the scar on her upper lip (ZA, segments [seg] 2 to 3) and the history pertaining to it. She revealed that she had suffered a dog bite when she was 11-years-old. Later, the patient had post-trauma lip surgery done to improve her cosmetic appearance (ZA, seg 2 and 3), but she was never satisfied with results. Finally, in her late 20s, the patient was informed that there was nothing that could be done for her remnant scarring. She was told that she would have to live with her lips as they were. Now in her late 30s, the patient explained to me in a resolved manner that she can live with her lips the way they are now, but would be open to other options in removing this painful memory that she sees everyday in her mirror. I explained that the potential treatment goal for correction was focused more on reestablishing symmetry and reduction than complete scar elimination.
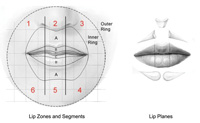 | 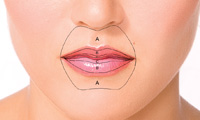 |
| Figure 1. Illustrated here are the zones and segments of the lip and perioral area. In addition, the planes make up the lips as a template for treatment procedures. | Figure 2. This is an illustration of the zones associated with the lip and perioral area. |
 |  |
| Figure 3. The patient at the initial visit: full face. | Figure 4. Notice the indurations of scar tissue in Zone A (ZA), segment (seg) 2 to 3. In addition, there is a slight asymmetry between the volume and lip architecture in ZA, seg 1 to 3. |
Clinically evaluation showed a 3- to 4-mm scar that is indurated producing a rhytid like appearance in ZA, seg 3. Examination also revealed a smaller, slightly indurated scar in ZA, seg 2, approximately 2 to 3 mm in vertical length. Both of these scars can be classified as mild to moderate in severity. Before treatment of any lip scar, or any scar for that matter, it is important to qualify it by its appearance and history. The techniques described in this case are for mild to moderate scars of the lip and perioral area (ZA, segments 1 to 6). MICPs, such as subcision, 7 can reduce scar severity significantly, immediately re-establishing a patient's cosmetic appearance. 8
In 1995, Orentreich 7 defined the procedure of subcision as a method of subcuticular undermining, using a tribeveled hypodermic needle, for the treatment of depressed cutaneous scars and wrinkles. The depression is lifted by the releasing action of the procedure, as well as from connective tissue that forms in the course of normal wound healing.
Subcision not only has a releasing effect, but also produces trauma at microscopic level within scar tissues. Newer matrix and collagen tissue is laid down, causing permanent clinical improvement in depressed rolling scars. Scar remodeling is a continuous process, and it cannot be considered to be in a steady-state until at least 2 years post-wounding. This may explain why results differ at 2 months and 6 months after subcision. In addition, it suggests 5% to 10% improvement is likely beyond 2 months. 9 It is important to realize that subcision techniques rarely resolve 100% of the scarring; the studies reveal that there is a decrease is scar appearance from 40% to 80%. 10
Noticing the mild to moderate extent of the scar, the nature of its presentation, and the scar history; I presented several treatment options to the patient:
Option 1: Simple dermal filler placement in contra lateral side (ZA, B seg 1 to 2).
Option 2: Subcision on scar in ZA, seg 1 to 2.
Option 3: Subcision, dermal filler placement, and fractional laser ablation in ZA, seg 1 to 3.
Our patient elected for treatment option 3. I then explained this may take 3 to 4 visits, each lasting about 20 minutes in duration. The treatments were to be spread out every week, or every other week, depending on patient healing. The final result would be realized after 2 to 3 months. The patient agreed.
Visit 1
 |  |
| Figure 5. This is an illustration of the Gordon Modified Block (GMB). The GMB is compared here to the conventional infra-orbital block. The GMB is targeted for the lip and perioral area, not affecting any tissue lateral to these borders. This reduces the unwarranted midface numb feeling that is often uncomfortable for patients. | Figure 6. This illustration shows the lancing motion of a 27-gauge tribevel hypodermic needle (12-mm) (B & G). The needle is inserted slightly below the dermis in ZA, seg 3. |
 |  |
| Figure 7. The technique calls for a sweeping and lancing motion in different directions underneath the scar tissue. | Figure 8. This illustration shows the same technique underneath the more medial scar in ZA, seg 2. |
Local anesthetic was (Lidocaine with 1:100,000 epinephrine) injected using the Gordon Modified Block (Figure 5). 11 In addition, 2 small buccal infiltrates were placed intraorally, 10 mm on the visualized occlusal plane of the buccal mucosal. This provides anesthesia for any lingering nerve innervations from the long-buccal nerve.
Figures 9 and 10. As illustrated, the vermilion border was entered in all locations of the various scars. During the procedure, the tissue is held above and around the targeted tissue for additional support.
A 27-gauge tribevel hypodermic needle (12 mm) (B & G) was used to separate subdermal attachments (also referred to as subcision). A lancing technique, and horizontal sweeping, was used to cut the fibrous strands beneath the scar tissue that were responsible for the indurated appearance (Figures 6 to 10). The clinician can actually tactilely feel the release of the adhesions throughout sweeping and lancing motions. For scars of this nature this is an extremely effective procedure with minimal trauma and swelling.

Figure 11 and 13. Dermal filler was injected underneath the undermined tissue for positive architecture, and to prevent immediate re-adhesion of dermis.
Immediately after subcision of the scar, an autogenous dermal filler was placed. In this case, cross-linked hyaluronic acid (Juvederm [Ultra, Allergan]) (Figures 11 to 13). The intended goal of immediate placement of dermal filler was to re-establish symmetry in ZA, seg 1; and to provide positive lip form architecture for ZA and ZB, seg 2 to 3. Studies suggest that a separation medium in the newly acquired space may assist in reducing the re-adherence or like cross linked hyaluronic acid stimulate collagen neogenisis. 12 Other separation mediums, such as cat gut, have been placed underneath subcision area techniques with no clinical significance. 13 Furthermore, it has been suggested that wound healing is influenced more by patient characteristic (such as age and gender or wound feature [ie, length and site]) than by using gut sutures. 14
Visit 2
Our patient returned to the office after one month with great results. She was happy and reported a significant re-duction in scar appearance. On a scale of one to 10 (10 being before we started, and zero total resolution of scar) , the patient reported a 4.
On the visit we decided to contimue treatment again for further resloution. Local anesthetic was applied similar to the initial visit. Additional subcision was performed on ZA, seg 1 to 3. During this treatment there were significantly less adhesions released in contrast to the initial treatment. A cold compress was applied and the patient was released.
Visit 3
 |  |
| Figure 14. This is the first postoperative photo of the patient, one week after the procedure. Notice the immediate resolution of the scars in ZA, seg 2 to 3. In addition, symmetry has been achieved by adding volume with dermal filler to Zone B (ZB) seg 1, and sculpting in ZA. | Figure 15. Photo after the second treatment session. Note the more sculpted look in the vermilion border of ZA, seg 1 to 3, and the symmetrical balance achieved. Laser treatment was then to be done to reduce scar elevation that was still present, and to create a more uniform skin appearance. |
On the third visit, the patient reported being at a 3 on her one to 10 scar revision scale (Figure 15). Patient's treatment results were evaluated at this point. We can see that induration of the scar has been dramatically reduced. We also have acquired symmetry in the upper lip ZA, seg 1 to 3. We still see an elevation of the scar in ZA, seg 2 and 3. It was discussed with the patient about laser therapy on her upper lip. The goal of this therapy was to induce remolding of the scar tissue and improve the overall comesis. It was explained that fractional laser treatment for the entire ZA would increase overall cosmesis of lip presentation. 15
Visit 4
 |  |
| Figure 16. The third visit was the laser treatment. The targeted area was ZA, seg 1 to 3. This photo shows the patient immediately after treatment. The slight whitish appearance of the lip is due to the ablated superficial dermis spots. (For purposes of photo illustration, safety glasses, mandatory for all laser applications, were taken off the patient) | Figure 17. Vinegar was used to remove this white area, with a quick application of topical petroleum jelly for a couple of days. |
 |  |
| Figure 18. The laser treatment was performed on the entire ZA, seg 1 to 3, in order to facilitate a harmonious tissue presentation and collagen remodeling. The slight redness around the treated area quickly subsided within a couple of hours post-treatment. Our patient was able to wear foundation makeup within a couple of days. | Figure 19. Ideal proportion, in regards to the upper lip to lower and the overall aesthetic value of the lips to the face, has been achieved. |
 |
| Figure 20. Final results: The patient is wearing a slight amount of makeup base and lip-gloss. Note lip symmetry in ZA seg 1 to 3. There is still a slightly longer and noticeable lip length in ZA and ZB, seg 2 to 3. However, compared to the preoperative look, a remarkable outcome has been achieved. |
Finally, 2 weeks later following subcision and dermal placement, fractional ablative laser therapy was performed in ZA, seg 1 to 3. 16 (Figures 16 and 17). The laser device used was the eCO 2 laser system (Lutronic). This is a CO 2 laser system that utilizes scanning technology to divide the laser energy into microscopic columns of light. The scanning technology used by this laser affects only a fractional percent of skin (5% to 40%), and the downtime is significantly less than traditional ablative resurfacing. Furthermore, it is a much safer modality of treatment. More notable is the important role of thermal heat induce by the microscopic light columns to effectively initiate immediate volumetric tissue reduction and new fibroblast activity to induce collagen stimulation for ongoing textural improvement. 17
The primary treatment goal in this clinical case was to relieve the scar tissue and to induce collagen remodeling, in and around the scar tissue itself. Fractional ablative laser treatment was selected.18 Since the scar was located in ZA, seg 2 to 3, it was treatment planned to laser the all segments of the upper lip to provide a uniform cosmetic appearance to the remodeled ZA (Figure 18). 19,20
The patient reported that her scar appearance was reduced from a 10 (at the beginning of treatment) to a 2 (after the end of treatment). (Figures 19 and 20).
DISCUSSION
The use of the subcision technique, in combination with dermal fillers provides satisfactory results in reducing/eliminating lip and perioral post-traumatic scar formation. It is also suggested that subcision and fraction laser therapy continues to remodel and produce cosmetic improvement up to 6-plus months after an initial procedure. 21 The actual procedure takes about 20 min chair time per session, with treatment duration lasting between 2 to 3 months. Select cases can be performed in the dental office with local anesthetic using minimal chair time.
Unfounded concerns arise from any new paradigm of treatment, and lip and perioral augmentation done by the cosmetic dentist is no different. What are some of the reactive concerns that the dentist may face in regards to these procedures? One concern, voiced by some professionals, is that they believe the dentist will soon be performing laser therapy throughout the whole body. Another concern is that dentists will soon want to begin doing facelifts, in addition to filling cavities. This author would like to address these concerns.
With the advent of minimally invasive cosmetic materials, equipment, and procedures, dentists are now able to treat conditions of the lip and perioral area (that may have previously required extensive surgical interventions) with significantly less traumatic/invasive alternatives. It is an evolution in the area of MICPs that have facilitated the mainstream dentist to offer treatment alternatives such as dermal fillers, Botulinum Neurotoxins, subcision, and fractional ablative laser within the area of their expertise. Most MICPs in North America are being performed by a broad spectrum of health practitioners. These include doctors, nurses, nurse practitioners, and physician assistants. It is the standard of care that is paramount across the various healthcare specialists that results in superior patient beneficence. We are ethically bound to do no harm, but at the same time we are obligated to maximize our training and knowledge base for our patients' benefits.
Dentists are tasked with the responsibility of cancer detection, wound management, and aesthetic smile design in the lip and perioral area. Either alone, or in cooperation with other healthcare practitioners of the oral facial area, dentists are considered to be the experts in treatment planning and differential diagnosis for optimal oral facial cosmesis.
CONCLUSION
This article has presented a clinical case that illustrates the use of minimally invasive techniques (subcision, dermal fillers, and ablative laser therapy) to correct and improve the cosmesis of post-traumatic scarring in the lip and perioral area. When properly trained, most cases like this can be performed the cosmetic dentist as an adjunct to their practice.
References
- Emshoff R, Schöning H, Röthler G, et al. Trends in the incidence and cause of sport-related mandibular fractures: a retrospective analysis. J Oral Maxillofac Surg. 1997;55:585-592.
- O'Neil DW, Clark MV, Lowe JW, et al. Oral trauma in children: a hospital survey. Oral Surg Oral Med Oral Pathol. 1989;68:691-696.
- Bauss O, Freitag S, Röhling J, et al. Influence of overjet and lip coverage on the prevalence and severity of in-cisor trauma. J Orofac Orthop. 2008;69:402-410.
- Robson F, Ramos-Jorge ML, Bendo CB, et al. Prevalence and determining factors of traumatic injuries to primary teeth in preschool children. Dent Traumatol. 2009;25:118-122.
- Shinya K, Taira T, Sawada M, et al. Facial injuries from falling: age-dependent characteristics. Ann Plast Surg. 1993;30:417-423.
- Klein AW. Soft tissue augmentation 2006: filler fantasy. Dermatol Ther. 2006;19:129-133.
- Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543-549.
- Klein AW, ed. Tissue Augmentation in Clinical Practice. 2nd ed. London, England: Informa Healthcare; 2005.
- Ferguson MW, Leigh IM. Wound healing. In: Champion RH, Burton JL, Burns T, et al (eds). Wound healing: Biological aspect of wound healing. Rook/Wilkinson/Ebling Textbook of Dermatology. 6th ed. Oxford, England: Blackwell Science; 1998:337-356.
- Vaishnani JB. Subcision in rolling acne scars with 24G needle. Indian J Dermatol Venereol Leprol. 2008;74:677-679.
- Gordon RW. Vermilion Dollar Lips. Tampa, Fla: Vermilion Dollar Publications; 2008.
- Wang F, Garza LA, Kang S, et al. In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Arch Dermatol. 2007;143:155-163.
- Balighi K, Robati RM, Moslehi H, et al. Subcision in acne scar with and without subdermal implant: a clinical trial. J Eur Acad Dermatol Venereol. 2008;22:707-711.
- Gabrielli F, Potenza C, Puddu P, et al. Suture materials and other factors associated with tissue reactivity, infection, and wound dehiscence among plastic surgery outpatients. Plast Reconstr Surg. 2001;107:38-45.
- Fulchiero GJ Jr, Parham-Vetter PC, Obagi S. Subcision and 1320-nm Nd:YAG nonablative laser resurfacing for the treatment of acne scars: a simultaneous split-face single patient trial. Dermatol Surg. 2004;30:1356-1359.
- Alam M, Levy R, Pajvani U, et al. Safety of radiofrequency treatment over human skin previously injected with medium-term injectable soft-tissue augmentation materials: a controlled pilot trial. Lasers Surg Med. 2006;38:205-210.
- Hantash BM, Bedi VP, Kapudia B, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:96-107.
- McDaniel DH, Lord J, Ash K, et al. Combined CO2/erbium:YAG laser resurfacing of peri-oral rhytides and side-by-side comparison with carbon dioxide laser alone. Dermatol Surg. 1999;25:285-293.
- Branson DF. Active rhytids and scars: enhancing the results of CO(2) laser skin resurfacing. Aesthet Surg J. 1998;18:36-37.
- Hedelund L, Bjerring P, Egekvist H, et al. Ablative versus nonablative treatment of perioral rhytides. A randomized controlled trial with long-term blinded clinical evaluations and non-invasive measurements. Lasers Surg Med. 2006;38:129-136.
- Orringer JS, Kang S, Johnson TM, et al. Connective tissue remodeling induced by carbon dioxide laser resurfacing of photodamaged human skin. Arch Dermatol. 2004;140:1326-1332.
Dr. Gordon graduated from Marquette University School of Dentistry and continued his education in a residency program in periodontics as well as additional oral/surgery training. He practices in Clearwater, Fla, and lectures often, instructing oral/facial augmenters on his classification, diagnostic, and reconstructive lip and perioral augmentation techniques. He can be reached via e-mail at dr.g@vermiliondollarlips.com or visit his Web site vermiliondollarlips.com for more information on his book, instructional videos, and learning seminars.
Disclosure: Dr. Gordon reports no conflicts of interest.
How to Get Rid of a Scar on Your Lip
Source: https://www.dentistrytoday.com/sp-1505107528/